Hysteroscopy Procedure
A hysteroscopy procedure is a minimally invasive method used to examine the inside of the uterus and, when needed, treat certain uterine conditions. It allows direct visual assessment of the uterine lining using a thin camera passed through the cervix. This helps diagnose abnormal bleeding, investigate fertility concerns and remove small abnormalities without abdominal surgery.
Many gynaecological symptoms originate from changes within the uterine cavity. Imaging tests such as ultrasound provide useful information, but direct visualisation offers greater clarity in selected cases. This approach enables both diagnosis and treatment in a single setting, improving accuracy and reducing the need for more invasive operations.
Why this examination is recommended
This investigation is commonly advised when a woman experiences heavy or irregular bleeding, bleeding after menopause or unexplained spotting between periods. It is also used when ultrasound findings suggest polyps, fibroids, thickened lining or retained tissue.
Women undergoing fertility evaluation or experiencing recurrent miscarriage may also benefit from direct assessment of the uterine cavity. Identifying structural abnormalities early can help guide further management and improve outcomes.
The procedure may serve either a diagnostic purpose, where the uterus is simply examined, or an operative purpose, where small instruments are used to remove growths or take tissue samples.
How long does a hysteroscopy take
Many patients understandably ask how long does a hysteroscopy take before planning their visit. A simple diagnostic examination usually lasts between 10 and 20 minutes. If treatment, such as removing a small polyp or taking a biopsy, is required, it may take slightly longer.
Although the examination itself is relatively short, the total time spent at the clinic may be longer. Preparation, explanation, consent and recovery monitoring are included within the appointment. In most cases it is performed as a day procedure, and hospital admission is not required.
What happens during the examination
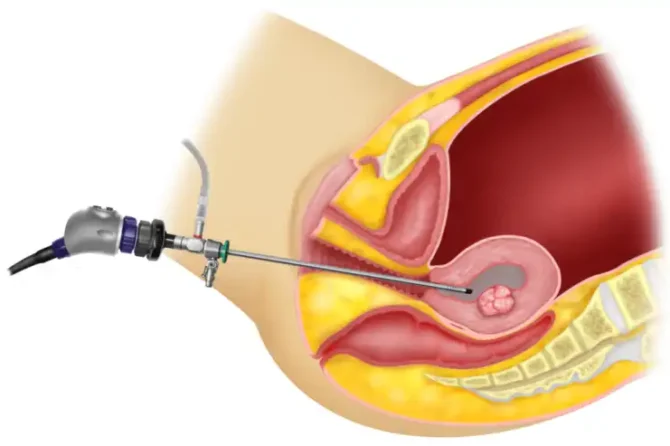
The process begins with positioning similar to a routine cervical screening test. A thin telescope called a hysteroscope is gently inserted through the cervix into the uterine cavity. No abdominal incisions are made.
Fluid is introduced to gently expand the uterus, allowing clear visualisation of the lining. The images are displayed on a monitor, enabling careful inspection. If abnormalities such as polyps or small fibroids are identified, fine instruments may be passed through the scope to remove them.
In some cases a small tissue sample may be taken for laboratory analysis. This helps confirm or exclude conditions affecting the endometrium.
Anaesthesia options vary depending on the reason for the examination and patient preference. Some women undergo the procedure with local anaesthetic, while others may require short general anaesthesia, particularly if operative treatment is planned.
Will treatment performed during the same visit
One of the advantages of this approach is the ability to treat certain problems immediately. Small polyps, adhesions or submucosal fibroids can often be removed during the same session.
Combining diagnosis and treatment reduces the need for multiple procedures. It also shortens recovery time compared with traditional surgical methods.
The decision to proceed with operative treatment depends on prior findings, symptoms and clinical assessment. In some situations diagnostic evaluation is performed first and treatment is scheduled separately.
Recovery and aftercare
Recovery is generally straightforward. Mild cramping, similar to period pain, is common for a few hours after the procedure. Light spotting may continue for several days.
Most women can return to normal daily activities within 24 hours. If sedation or general anaesthesia was used, driving and strenuous activity may need to be avoided temporarily.
It is important to seek medical advice if heavy bleeding, severe pain, fever or unusual discharge occurs. These symptoms are uncommon but require prompt review.
Is a hysteroscopy a major surgery
No, it is not considered major surgery. It does not involve abdominal cuts, stitches or prolonged hospital stays. The technique is classified as minimally invasive and is usually performed as a daycase procedure.
Because the uterus is accessed through the natural cervical opening, recovery tends to be quicker than traditional open surgical approaches. Most women resume normal routines within a short period.
Is it painful to have a hysteroscopy
Pain levels vary from person to person. Some women experience mild discomfort or cramping, similar to menstrual pain, during the procedure. Others report only brief pressure sensations.
When treatment is performed at the same time, discomfort may be slightly greater. Pain relief options are available and can be discussed beforehand. Most women find that any discomfort settles soon after the examination is completed.
Benefits of direct uterine assessment
Direct visualisation provides precise information about the uterine lining. It helps confirm diagnoses that cannot always be established through imaging alone.
The ability to both diagnose and treat conditions in a single visit reduces delays in care. It also minimises the need for more invasive surgical procedures in many cases.
For women experiencing persistent bleeding, fertility concerns or abnormal findings on ultrasound, this method offers clarity and targeted management.
This minimally invasive examination plays an important role in modern gynaecology. It allows accurate evaluation of the uterine cavity and enables treatment of certain conditions without major surgery. With short procedure times and relatively quick recovery, it provides an effective option for diagnosing and managing common uterine concerns.
If you have symptoms such as abnormal bleeding, irregular cycles or fertility concerns, you can book an appointment with our doctor at Ovara Health for personalised assessment and guidance regarding appropriate investigations.